-
Learn about REMICADE®
- Adult: moderately to severely active Crohn’s disease
- Pediatric: moderately to severely active Crohn's disease
- Adult: moderately to severely active ulcerative colitis
- Pediatric: moderately to severely active ulcerative colitis
- Adult: moderately to severely active rheumatoid arthritis
- Adult: active psoriatic arthritis
- Adult: active ankylosing spondylitis
- Adult: chronic severe plaque psoriasis
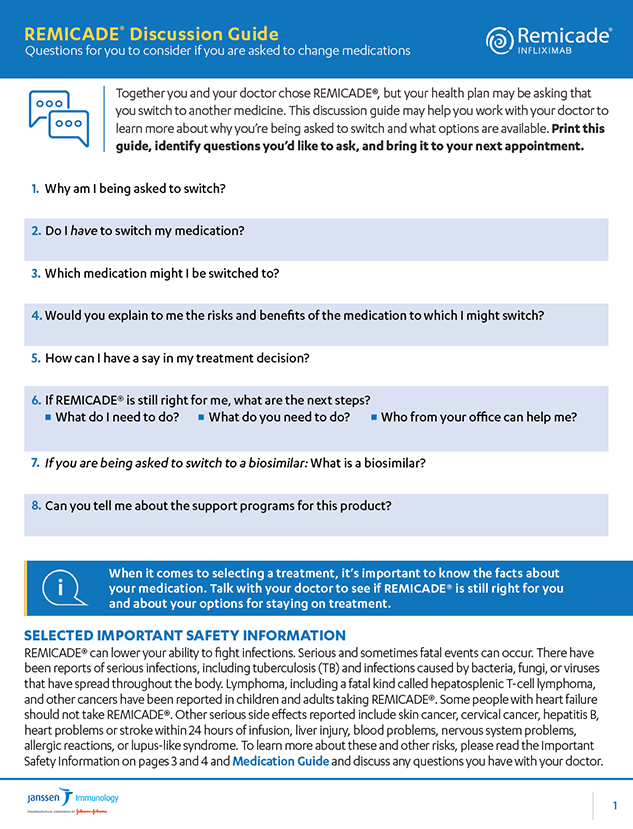
- Continuing on REMICADE®
-
The infusion process for REMICADE®
- Adult: moderately to severely active Crohn’s disease
- Pediatric: moderately to severely active Crohn's disease
- Adult: moderately to severely active ulcerative colitis
- Pediatric: moderately to severely active ulcerative colitis
- Adult: moderately to severely active rheumatoid arthritis
- Adult: active psoriatic arthritis
- Adult: active ankylosing spondylitis
- Adult: chronic severe plaque psoriasis
- Cost support & more
- Additional resources